
7 Healthcare Workflows That Can Be Automated To Improve Patient Care
.jpg)
If you're leading tech, product, or focusing on healthcare operations improvement, chances are you’re no stranger to broken workflows.
Teams are juggling outdated systems, duplicating data entry, and relying on memory to manage patient handoffs. What should be temporary workarounds often become permanent fixtures.
So the question isn’t whether change is needed.
It’s: Where do you start?
Can You Improve Without a Complete Overhaul?
Absolutely.
A full rebuild sounds promising, but it’s rarely practical. We’ve worked with teams that spent months scoping migrations, building roadmaps, and specifying out all-in-one systems—only to hit roadblocks in rollout, change management, or budget.
In most cases, the faster, more realistic path is this: start with one high-friction workflow. Something repetitive. Error-prone. Delay-heavy.
You don’t need to fix everything at once; you just need to improve what’s underperforming.
Why Healthcare Workflow Automation Matters
Repetition kills efficiency.
And healthcare is full of it: onboarding, scheduling, insurance checks, discharge… It’s the same rinse-and-repeat cycle, all day. Manual work isn’t just slow; it invites mistakes. Even a single missed form field can cause delays, follow-ups, and unnecessary friction.
Automating healthcare workflows solves that. Not by replacing people, but by reducing paperwork or speeding up repetitive tasks with healthcare workflow software and healthcare automation tools. At its core, it’s about unlocking capacity. Staff are freed from low-value tasks, patients receive a smoother experience, and administrators gain better oversight and control.
The Real Cost of Doing Things Manually
We’ve all seen it happen.
Every time you depend on someone to remember the next step, something slips.
And sure, it may not be critical at first. But over time, those small breakdowns accumulate. In healthcare, staff burnout. In lagging reimbursements. In patients having to explain the same thing three different times to three different people. In fact, a growing body of research shows that administrative overload is a leading cause of healthcare staff burnout among professionals.
When workflows lean entirely on memory, we leave too much to chance.
And in healthcare, that’s not a luxury anyone has.
How to Prioritize Which Workflows to Automate First
You don’t need to automate everything at once. Start with what’s most likely to deliver fast, measurable improvements. In general, the best candidates for early automation are workflows that are:
👉 High volume
👉 Low to moderate complexity
👉 Prone to delays or manual errors
From there, work with cross-functional teams to validate the needs, assess the impact, and ensure user buy-in. A phased approach, with testing and feedback loops, is often the most effective and least disruptive path.
Now that we’ve discussed why automation matters, the hidden costs of manual work, and how to prioritize your rollout, it’s time to dive into specifics. The next section highlights seven healthcare workflows that are common across organizations and have shown measurable improvements through healthcare process automation.
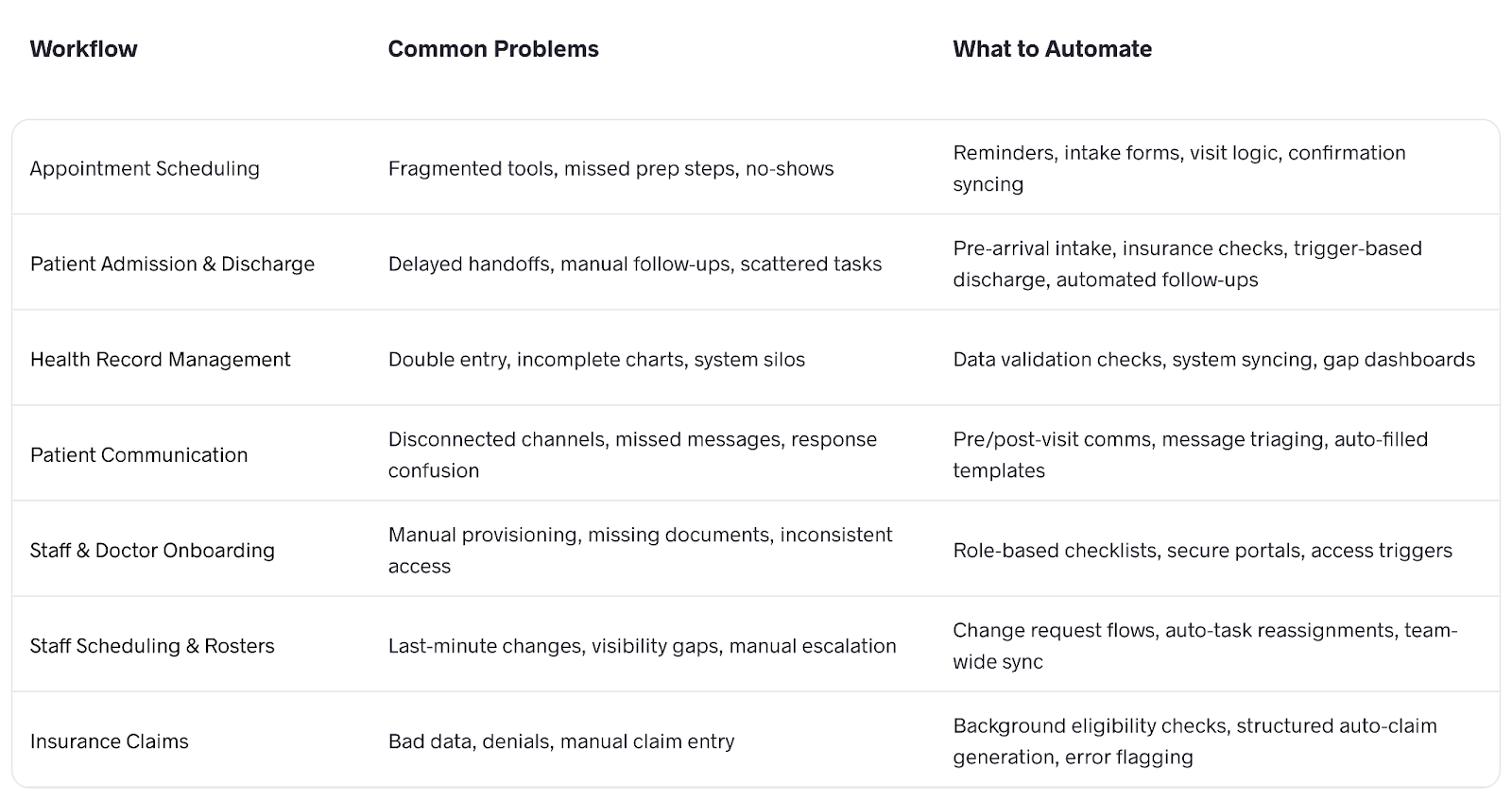
Workflow Automation Cheat Sheet
Top 7 Healthcare Workflows to Automate
1. Appointment Scheduling
Most scheduling systems are fragmented. Even with online booking tools, key logic like provider availability, visit types, and prep instructions is often missing or loosely enforced.
You don’t need to build a new app to fix this. Start by identifying your most common appointment types: new patients, follow-ups, referrals, and define the rules around each.
Then automate the basics:
- Confirmations
- Reminders
- Pre-visit intake
Lightweight solutions that integrate with your EHR or CRM are often enough. What matters is ensuring schedules sync across departments and reflect operational constraints like staff availability and room usage.
2. Patient Admission & Discharge
Admissions and discharges often depend on slow handoffs between departments: registration, nursing, pharmacy, and billing. When each one relies on manual follow-ups or phone calls, the entire process stalls.
Here’s what automation can fix:
Pre-arrival intake: Let patients complete demographics, consent forms, and insurance uploads online before arrival. This information should feed directly into the EHR, removing double entry at the front desk.
Real-time eligibility checks: Set up automated insurance verification as soon as a patient registers. This avoids hold-ups later when claims are submitted.
Trigger-based discharge workflows: Configure your system so that when a physician updates a patient’s status to “discharge planned,” it automatically notifies pharmacy, generates billing drafts, and sends discharge instructions to the nurse, without waiting for a coordinator to step in.
Automated follow-ups: Once discharged, the system schedules post-visit check-ins, sends summaries to patients via the portal/email, and flags any incomplete documentation for review.
The goal isn’t just to speed things up. It’s to reduce reliance on memory and manual tracking. When next steps are automated, nothing gets missed, and the entire process becomes more reliable.
3. Health Record Management
Most healthcare organizations have an EHR. But in practice, it rarely works well with the rest of the system.
Lab results arrive by email. Intake forms are scanned and uploaded. Notes get typed twice—once on paper, again into the record. It’s a disjointed workflow that forces clinical teams to act as system integrators.
If your team is spending more time reconciling systems than delivering care, it’s time to intervene.
The good news is, you don’t need to replace your EHR. You just need to make it work better with the tools around it.
What you can do:
- Catch missing data automatically
Set up checks that flag incomplete fields. If vitals weren’t logged or allergy history is missing, staff get alerted right away, before it turns into a bigger issue.
- Cut down on double entry
Use scripts or basic integrations to sync data between systems. Intake forms, lab results, and notes shouldn’t have to be entered more than once.
- Make gaps easy to see
A simple dashboard that pulls up incomplete or outdated records helps your team stay ahead without digging through charts.
4. Patient Communication
Most clinics already have tools for patient communication. The real issue is that they’re rarely connected.
You might have calls, texts, patient portals, and shared inboxes—all running in parallel, with no clear record of who said what, when, or through which channel.
Fixing this starts with better infrastructure. Identify clear automation points across the patient journey:
- At scheduling:
Send pre-visit instructions, intake forms, and location-specific details. - Before the visit:
Trigger reminders through the patient’s preferred channel: text, email, or app. - After the visit:
Automate follow-ups like visit summaries, feedback requests, and next steps.
Each message should pull directly from your EHR or CRM. That way, the patient’s name, provider, visit type, and instructions are filled in automatically, without relying on someone to edit a template.
One more critical step: route replies to the right place. If a patient responds with a billing question, it shouldn’t end up with the nurse. Use automation to triage messages by topic so that each team only sees what’s relevant.
Every time you rely on someone to "remember to follow up," you create a gap. And most clinics are still operating that way, even with the right tools already in place.
5. Staff & Doctor Onboarding
You’ve finally hired the right nurse practitioner after weeks of searching. But on day one, they’re stuck waiting—no EMR access, no badge, no email. Half their documents are still buried in someone’s inbox.
The problem is the fragmented coordination across HR, IT, compliance, and operations. When onboarding is scattered, so is accountability.
Automation closes the gap between “hired” and “ready.”
- As soon as someone signs the offer, trigger a checklist based on their role. It outlines exactly what needs to be submitted, completed, or reviewed before their first day.
- Use a secure portal to collect documents like licenses, IDs, and background checks. The system should validate uploads automatically and send reminders when something’s missing.
- Tie onboarding progress to system access. Complete the compliance module and get EMR access. Submit the license and gain provisioning access.
If your process still depends on reminders, spreadsheets, or memory, something will eventually slip through. Automating onboarding doesn’t just make things faster. It makes them consistent. That consistency reduces risk, avoids delays, and lets new hires contribute from day one, not week two.
6. Staff Scheduling & Rosters
For many healthcare organizations, staff scheduling remains a surprisingly manual process, despite advances in healthcare workflow automation tools. Outdated tools, department-specific workarounds, and reactive adjustments make it difficult to maintain consistency. Teams often rely on patchwork fixes—until a sick call, shift conflict, or mid-week breakdown exposes the gaps.
Most teams don’t need a full rebuild. Using a structured tool like Google Calendar, combined with a proper change request flow, is often enough to restore visibility and prevent escalation loops.
More importantly, when changes happen—as they inevitably do—the system can reroute tasks, notify pre-cleared replacements, and adjust workload distribution across teams. That means fewer downstream disruptions and fewer handoffs that fall through the cracks.
7. Insurance Claims
Claim denials usually trace back to bad or missing data, often due to gaps that go unnoticed until it’s too late. And the longer it takes to catch, the more expensive it becomes.
Start at intake. Eligibility checks should run in the background as soon as an appointment is scheduled. When the visit wraps, claims should auto-generate using structured data from the EHR. If anything’s missing or inconsistent, the system flags it immediately. You want errors caught before submission, not after denial.
Measuring Success and Continuous Improvement
Workflow improvement requires consistent monitoring. As teams and priorities evolve, even strong systems can become less effective.
Tracking performance indicators such as task completion times, error rates, staff satisfaction, and patient feedback provides a clear view of what is working and what needs adjustment.
Regular review cycles help keep track of improvements. They reinforce a culture of continuous refinement rather than allowing teams to settle into outdated habits. Feedback from frontline staff is especially important to ensure updates reflect real-world needs.
Final Thoughts
You can’t scale innovation if your operations don’t scale with you.
Even the best product roadmap or care model won’t reach its potential if basic workflows are still being held together manually.
We’ve seen teams try to fix these problems by launching new systems, adopting all-in-one platforms, or spinning up rebuild projects that never ship.
In most cases, that’s not necessary. You don’t need a six-month roadmap or a major platform migration to get started. We work with healthcare teams to identify one high-friction workflow and modernize it end-to-end, with a dedicated product team that runs in parallel to your day-to-day ops.
If you’re stuck figuring out where to begin, we’re happy to help spot the easiest win.

.png)
.avif)

.jpg)
.avif)
.avif)